Provided and edited by the members of the MARI authors; Iman Khalid, Lovepreet Singh, and Pooya Beigi MSc.MD.
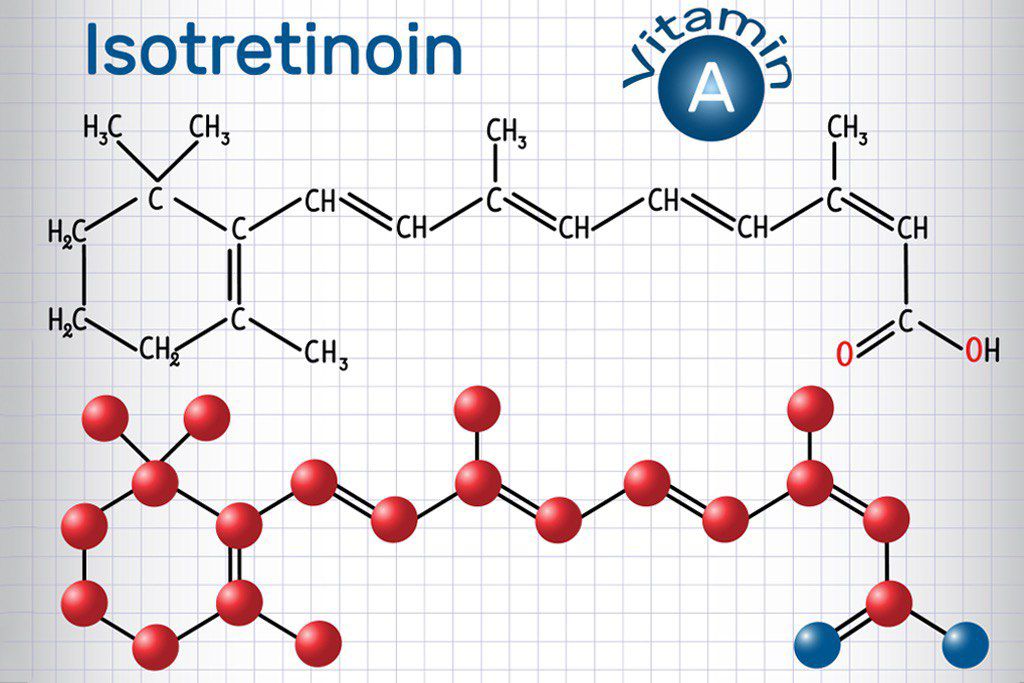
WHAT ISOTRETINOIN IS AND WHAT IT IS USED FOR
Isotretinoin (also known as Roaccutane) belongs to a group of medications known as retinoids which are derivatives of vitamin A. It is used to treat severe acne such as nodular or conglobate acne, or acne that is at risk of causing permanent scarring. This drug works by targeting sebum and keratin production, both of which are involved in the development of acne.
Isotretinoin may also be used to treat hidradenitis suppurativa and rosacea. In the UK, isotretinoin is only prescribed if the patient is being seen by a consultant dermatologist (an experienced doctor who speci alises in the treatment of skin, hair and nail conditions).
A significant improvement in acne symptoms is seen in 90% of those who take isotretinoin. However, some may still experience milder acne symptoms after finishing a course of isotretinoin but this can be treated using other medications including antibiotics.
WHAT YOU NEED TO KNOW BEFORE YOU TAKE ISOTRETINOIN CAPSULES
Do not take Isotretinoin Capsules if:
you are pregnant, think you may be pregnant or are breast-feeding – if there is any chance you could become pregnant, you must follow the precautions under “Pregnancy and prevention programme”
- You are allergic to isotretinoin, peanut, soya or any of the ingredients in Isotretinoin capsules
- You have liver disease
- You are taking certain antibiotics called tetracyclines
- You have very high levels of vitamin A in your body (Hypervitaminosis A) or are taking vitamin A supplements
- You have very high levels of cholesterol or triglycerides (a fat like substance) in your blood.
Approach with caution if:
You have peanut or soya allergies – those allergic to peanut or soya rarely experience an allergic reaction to isotretinoin. This will need to be managed by the dermatologist or pharmacist.
Women who are pregnant must not take Isotretinoin Capsules This drug is dangerous to the unborn baby – it can lead to intellectual disability and other serious complications. It also increases the risk of miscarriage.
Therefore:
- You must not take Isotretinoin if you are pregnant or if you think you may be
pregnant. - You must not take Isotretinoin if you are breast-feeding. The medicine is likely
to pass into your milk and may harm your baby. - You must not take Isotretinoin if you could get pregnant during treatment.
- You must not get pregnant for one month after stopping this treatment as trace amounts of the medication may still be in your bloodstream The Pregnancy Prevention Programme This is a programme designed by the government and the Medicines and Healthcare products Regulatory Agency for women who are of child-bearing potential to lower risk of pregnancy. Women of child-bearing potential must be on at least one (but preferably two) effective contraception methods.
This includes:
The combined oral contraceptive pill (however, the oral progesterone pill is not effective enough to be used by itself but can be used with other methods) Barrier methods – including condoms and caps. However, they should not be used alone and must be used together with other methods Isotretinoin is then started after a negative pregnancy test at the clinic, ideally starting on day 2 or 3 of your menstrual cycle. A pregnancy test will be carried out at the clinic each month, with the final one done 5 weeks after treatment has finished. Contraceptive methods must be continued for a month after treatment stops.
Those who may be exempt from this programme include:
Those who have undergone a hysterectomy
Those who are post-menopausal
Those who are unable to fall pregnant due to other medical conditions
In some cases, those who are not sexually active may qualify to be exempt from this programme. If you get pregnant whilst taking Isotretinoin or one month after finishing treatment, stop taking the medicine straight away, and contact your doctor. Your doctor may send you to a specialist pregnancy clinic, where a termination of pregnancy may be recommended.
Issues with Mental Health One of the rare side effects of taking Isotretinoin is changes to mood. This may sometimes include thoughts of self-harm and suicide. A history of low mood, depression or suicidal thoughts may increase the risk of experiencing these side effects, so it is vital to disclose this to your dermatologist. If needed, the dermatologist will ask a psychiatrist to meet with you before initiating Isotretinoin treatment.
HOW TO TAKE ISOTRETINOIN CAPSULES
Always take this medicine exactly as your doctor or pharmacist has told you to.Isotretinoin should be taken after a meal to help with absorption and must be swallowed whole. Most people take 20-80mg a day for 16-24 weeks, but the dose is individualised to each patient and some may have to take it for longer. During subsequent appointments, the dose may also have to be changed. Check with your doctor or pharmacist if you are unsure of your dose.
Most patients only need one course. For a few patients, the acne may get worse during the first 7- 10 days of treatment. Your acne should improve with continued treatment and may continue to improve for a few months after completion of the treatment
course
POSSIBLE SIDE EFFECTS
Stop taking the capsules and contact your doctor IMMEDIATELY if any of the following occur:
serious skin rashes (erythema multiforme, Stevens-Johnson syndrome, and toxic epidermal necrolysis), which are potentially life-threatening and require immediate medical attention. These appear initially as circular patches often with central blisters usually on arms and hands or legs and feet, more severe rashes may include blistering of the chest and back. Additional symptoms such as infection of the eye (conjunctivitis) or ulcers of the mouth, throat or nose may occur.
- Symptoms of a severe allergic (hypersensitivity) reaction such as wheezing or difficulty in breathing, swelling of face, tongue or throat, itching, rash
- Muscle weakness which can be potentially life-threatening, may be associated with trouble moving arms or legs, painful, swollen, bruised areas of the body, dark-coloured urine, reduced or no urine output, confusion or dehydration.
- Persistent headache, nausea, vomiting and blurred vision.
- Dry eyes, sight problems, colour vision disturbances or reduced night vision.
- Yellow skin or eyes and feeling tired.
- Difficulty urinating (passing water), swollen and puffy eyelids, feeling excessively tired.
- Sudden tight chest, shortness of breath and wheezing, particularly if you have asthmaI

Common side effects (may affect up to 1 in 10 people):
Dryness of the skin, lips, and eyes – use lip balm, eye drops and moisturiser that does not clog the skin pores to help manage this
- Headaches
- Increased blood cholesterol
- Changes in blood glucose levels especially in diabetics
- Blood or protein in the urine
- The inside of the nose may become dry and "crusted", which may lead to mild nosebleeds. Applying a thin layer of petroleum jelly gently to the inside of the nose will help
- Sore or inflamed throat and nose.
- Uscle and joint ache after exercise
- Temporary hair thinning
Rare side effects (1 in 1,000 to 1 in 10,000 people):
Difficulty with night vision – if this develops, avoid driving and operating heavy machinery
Low mood
Increased pressure in the brain – causes severe headache, nausea, vomiting and blurred vision
Erectile dysfunction, vaginal dryness, decreased libido
Developing Inflammatory Bowel Disease – stop taking medication immediately if you develop bloody diarrhoea
Other cautions:
Do not share medication with others
Do not donate blood whilst on isotretinoin and for one month after finishing treatment
Do not exceed 14 units of alcohol a week
Let the dermatologist and pharmacist know of any other medications you are taking
Avoid taking tetracycline antibiotics, methotrexate and vitamin A supplements.